How does the VA support the nearly half of veterans who are 65 and older?
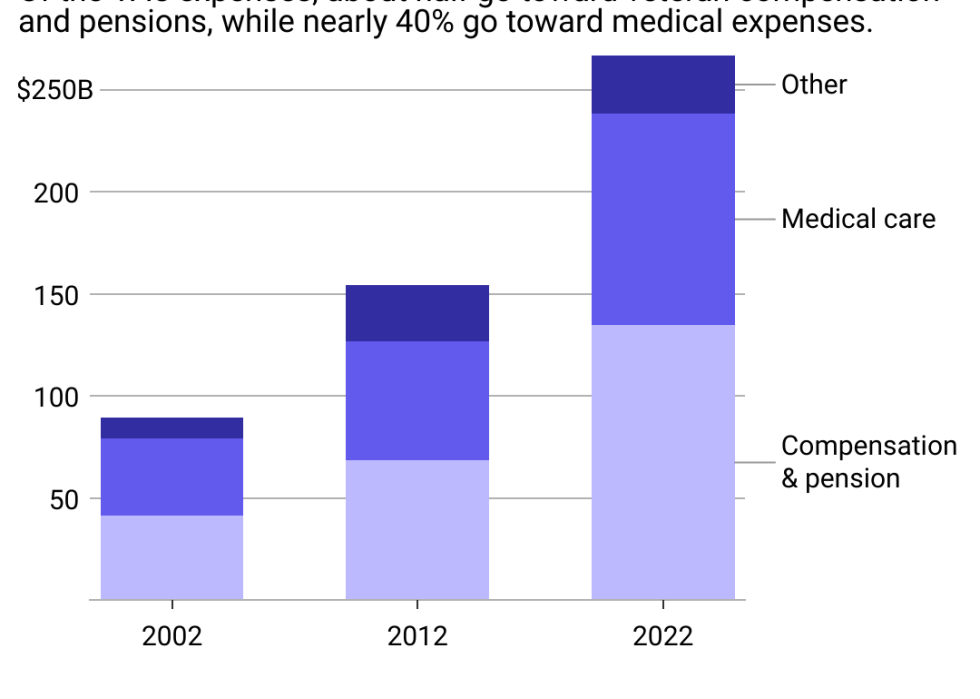
After steady growth over the past 20 years, VA expenditures surpassed $266.7 billion in 2022. The agency received a budget of $303.2 billion in 2023, including record-high discretionary funds.
The largest expense category is compensation and pensions, which largely represent monthly payments to retired service members and their families. The share of veterans receiving disability compensation, in particular, has nearly tripled over the past two decades, as has the average annual benefit paid out to those veterans, according to a Standford Institute for Economic Policy Research analysis.
Disability compensation is paid to veterans with disabilities and medical conditions that were caused or worsened during their service, and new research has broadened eligibility criteria. For instance, veterans with diabetes who were exposed to Agent Orange are now eligible for disability compensation, as researchers identified the herbicide as a risk factor for the disease.
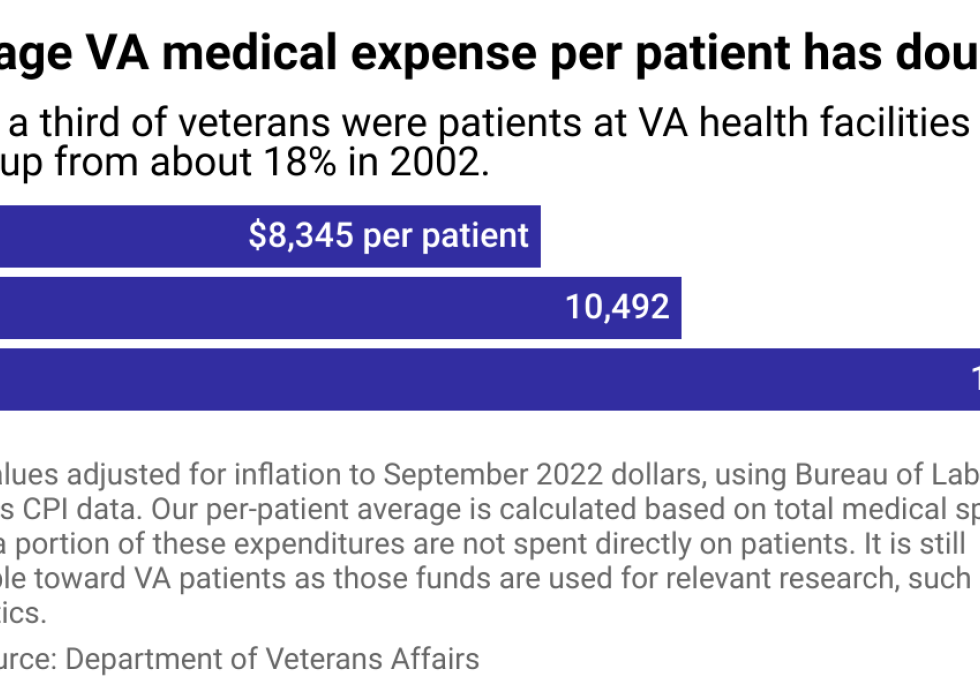
Medical care is the other dominant VA expense. About 38% of veterans are enrolled in VA health care—with slightly higher rates among those over age 65. Health benefits through the VA are typically more affordable for veterans. They have diversified in recent years, particularly in maternal and reproductive health care. The VA has also grown mental health services, including emergency medical care for veterans in suicidal crises.
These health care expansions have been vital, as the VA reports that veterans enrolled with the VA have better health outcomes than those who are not.
Nearly half of U.S. veterans were 65 years or older in 2021, compared to about 17% of the general population, Census Bureau data shows. This age group accounts for 36% of U.S. health spending as older adults tend to develop health conditions and disabilities that require costlier care. For veterans, those trends are even more pronounced. For instance, about a third of the general 65-plus population is disabled, while about 42% of veterans in that age bracket are disabled.
More than 100 VA medical centers have committed to providing holistic care for aging veterans by participating in the official Age-Friendly Health Systems movement. This movement centers around older patients' care preferences, including end-of-life care, using medications that don't interfere with elders' priorities, retaining mobility, and preventing or managing common mental health conditions that come with age, like depression and dementia.
Participation in the VA's medical program has grown along with the rising number of older veterans. Paired with rising health care costs more generally—the cost of medical care in the U.S. doubled from 2002 to 2022—VA expenses ballooned as the organization provided veterans with the health care necessary to maintain or improve their quality of life.
Despite the rise in expenditures, costs will ebb as the number of living veterans from major military campaigns—including World War II, Korea, and Vietnam—decreases overall. Today, the U.S. military has about 1.3 million active-duty troops—down from about 3.5 million in 1968. Over time, this decline should temper VA spending, even while retaining or improving the quality of care and benefits for surviving veterans.
Story editing by Nicole Caldwell. Copy editing by Kristen Wegrzyn.
